Women Connect

Pain Points: Online Resources
To ensure you have this important information at your fingertips, we're providing eco-friendly online resources from our Women Connect "Pain Points" chronic pain event.
We appreciate everyone who made time to join us for our expert Q&A, free flu shots, exercise class and more!
A special thanks to our expert panelists:
- Alicia Birky, MPT – Physical Therapist, Methodist Hospital
- Dr. Jery Inbarasu – Physical Medicine and Rehabilitation, Methodist Physicians Clinic HealthWest
- Dr. Carolee Jones – Obstetrics and Gynecology, Methodist Physicians Clinic Women's Center
The information shared below is meant for education and general guidance. Everyone’s experience with pain is different, so please talk with your health care provider before starting or changing any treatment or exercise plan.
Takeaways from Our Expert Q&A
-
Acute pain typically comes on suddenly, often after an injury, surgery, or illness. It’s your body’s warning signal that something’s wrong and healing needs to happen. Usually, as the tissue heals, the pain improves and eventually goes away.
Chronic pain, on the other hand, lasts longer than the normal healing period, generally more than three months.
With acute pain, the discomfort tends to stay localized, limited to the specific area that was injured. But with chronic pain, the pain might spread beyond the original site, or the person’s threshold for pain may decrease. Those can be signs that the pain has shifted from an acute process into something chronic.
Pain isn’t just physical; it can take a real emotional toll, too. That’s why it's important to take a comprehensive approach that goes beyond medication. Managing chronic pain can also involve therapy, movement, stress management and social support.
Alicia Birky, MPT, compares pain to an onion with many layers. At the core, there is a real physical injury, but around that, layers start to form: frustration, fear, blame and sometimes strained relationships. That’s where support systems matter, whether it’s family, friends, a therapist or a support group.
It’s also important to look at self-treatment habits. Sometimes, people cope by overusing social media, isolating themselves or turning to alcohol — things that might give short-term relief but can actually make things worse in the long run. Building healthier routines, staying connected, and finding small wins each day can make a big difference in how you manage pain physically and emotionally.
Increase your knowledge.
When you start to really understand what’s happening in your body, you can also start to untangle some of the fear that comes with pain. A lot of those fears are based on misunderstandings — that moving will make things worse or that pain always means damage. The more you learn, the more you can challenge those assumptions.
Alicia Birky, MPT, says that understanding the psychology of pain is a big part of that. It takes away some of the fear and empowers you to be the captain of your own "health ship." She recommends the book Explain Pain as a resource — a way to better understand the science behind how your brain and body interpret pain. You can download it for free here.
Set meaningful, realistic goals.
Dr. Jery Inbarasu says, "When I work with patients, I ask what’s most important to them — what helps them feel like themselves and what brings meaning to their lives. Then we talk about how to bring some of that back, even in small ways. It doesn’t have to be all or nothing. Some is better than none. Set realistic, meaningful goals and then determine the most logical way to get there."
Move.
Dr. Carolee Jones stressed the importance of movement. That doesn’t mean running marathons or spending hours at the gym. It means gentle, consistent movement in whatever way your body allows. "It could be just getting up and stretching or getting in the shower," she said.
Even small motions help keep your muscles active, your joints flexible, and your mind engaged. "Try to achieve those reasonable goals every day and ask, 'What else can I do today?'"
Alicia Birky, MPT offered this advice: "Start by thinking about what you want to be able to do. For one person, that might be walking comfortably around the block. For another, it might be squatting down to pick up a child, or being able to clean the house without needing to rest every few minutes.
"It’s helpful to know what your end goal is because that guides everything else. In physical therapy, we look at all the movements that go into that goal — things like balance, bending, reaching, twisting or getting up and down from the floor — and then we build strength and flexibility in those specific areas.
"If you’re working on your own, start by breaking that activity down. What's the activity that I want? How much of it can I do right now that is pain-free? Can I walk 5 minutes without pain? Then, I want you to walk every day for 5 minutes. After a week or two, try 6 minutes."
Set specific, realistic goals for yourself and be consistent. Over time, those small, safe, intentional steps can add up to real progress.
Note: If new or worsening symptoms occur (numbness, weakness, red-flag signs), stop and contact your clinician.
Dr. Carolee Jones: "It's a two-way street. You need to advocate for yourself, but you also need to be open to trying different strategies to manage the pain. If I feel as though I'm not addressing your pain, I'm going to try and refer you to someone who might be able to help. That multi-disciplinary approach — bringing together different specialties and perspectives — tends to help patients much more than simply relying on pain medication alone.”
Dr. Jery Inbarasu: "When we first see someone with pain, part of our job is to make sure there’s not a serious or progressive condition that could cause problems down the road if it’s not treated properly. That’s always one of our first goals. As we work toward finding the right diagnosis, it helps to remember that your care team is made up of humans; we’re doing our best to understand what you’re feeling, even though we can’t feel it ourselves. Open communication is key. The more specific you can be about your pain — when it happens, what makes it better or worse — the more we can fine-tune the treatment plan."
Resources to help you feel your best!
We all experience pain. What happens when it doesn't go away? We pulled together articles from our Methodist experts to help you find some relief.
As always, when it comes to you and your health, speak with your doctor about what’s best for you.
- If you need a primary care provider, visit BestCare.org.
- Learn more about:
- If you need a licensed mental health practitioner, Methodist Community Counseling Program provides accessible and affordable behavioral health care where you live, work and learn. For more information, visit MCCP's website.

Methodist Offers Energy-Based Healing Touch Program To Reduce Pain and Increase Relaxation
Methodist's Healing Touch program offers a nonpharmacological approach to pain management that Methodist offers.
The gentle, nurturing, compassionate form of energy therapy aims to complement the body’s natural ability to heal.

Nagging Aches and Pain Got You Down? Here’s What to Do About Them and When to Seek Help
While there’s not always a cure for chronic pain conditions, recognition and proper treatment can significantly improve your quality of life and functionality.

10 Tips to Prevent Pain From Using Phones, Computers and Other Devices
It can seem like you have a phone, tablet, computer or electronic device in your hands almost every minute of the day. The portability of these devices allow for endless positioning options when using them.
Over time, the resulting loss of body awareness and repeated motions can result in poor posture, aches, pains and even injury to the hands and upper extremities.

5 Solutions for Your Teen's Painful Periods
When a young woman starts her cycle, it’s not always easy. Relatively few teenagers have normal, regular periods when they first begin.
One of the most frequent things we see in younger patients is very heavy, painful periods. It all has to do with hormones and getting the brain and body working in sync.
Resource for you
Free Download: Explain Pain
During our Q&A, our experts referenced the book Explain Pain by David Butler and G. Lorimor Moseley.
Explain Pain unpacks the fascinating science behind how your brain and body interpret pain. Written in clear language, it drives home the point that pain is real, but not always a sign of damage — and that knowledge can be a powerful step toward healing.
Download your free copy of Explain Pain to take control of your recovery and learn practical ways to retrain your body and brain.
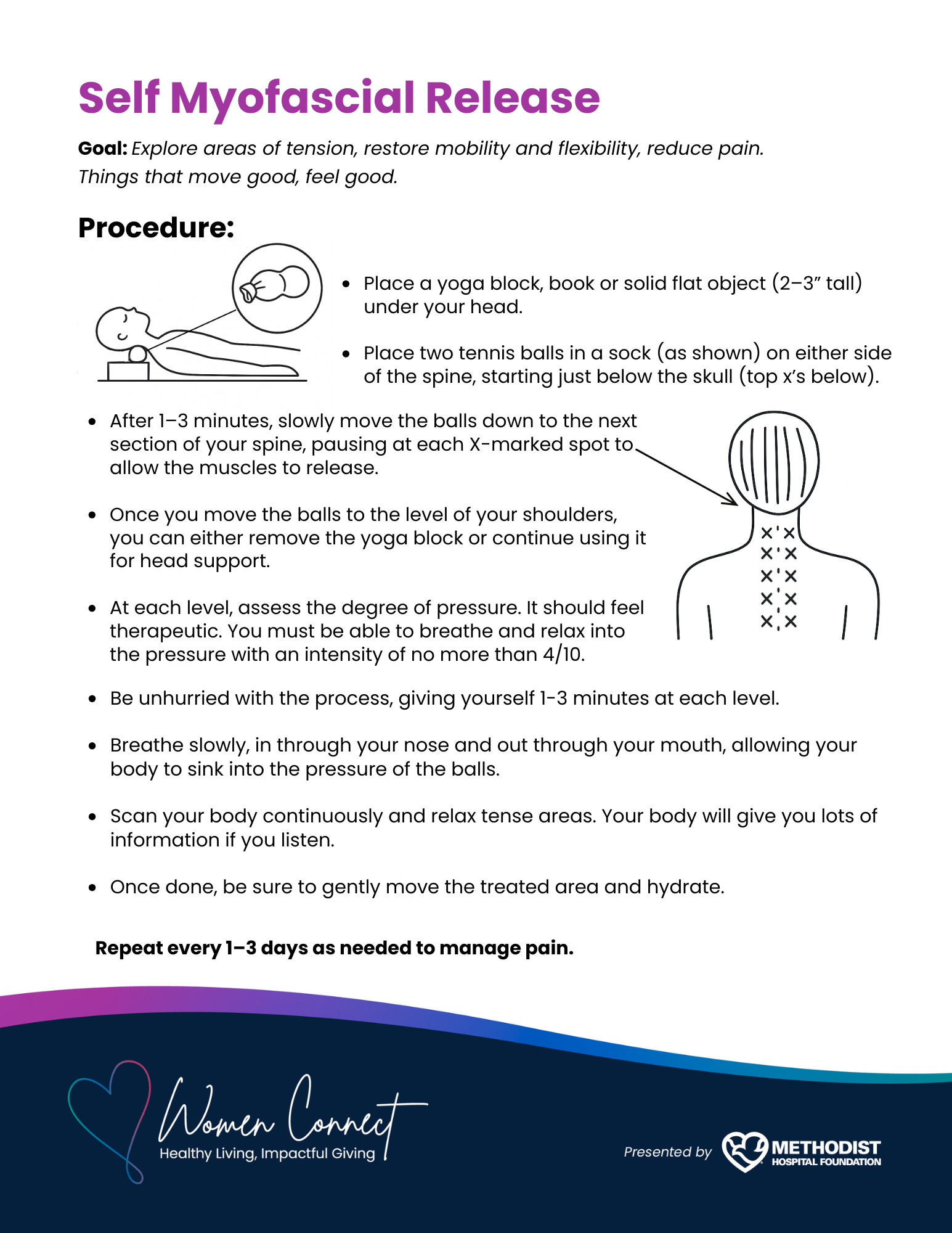
Self Myofascial Release
This activity is designed to help you explore areas of tension, restore mobility and flexibility, reduce pain. Things that move good, feel good. Click on each image below for instructions on how to complete the exercises.
Harper's Hope | Physical wellness classes for cancer survivors
Did you know you don't have to be a Methodist patient to take advantage of the Harper's Hope Cancer Survivorship Program and the physical wellness classes it offers? The classes are open to all of our community's cancer survivors.
There is a small fee to participate in the physical wellness classes. Payment can be made in person or online. Financial assistance is available through Methodist Hospital Foundation. No one is turned away due to an inability to pay.
Click here for more information.
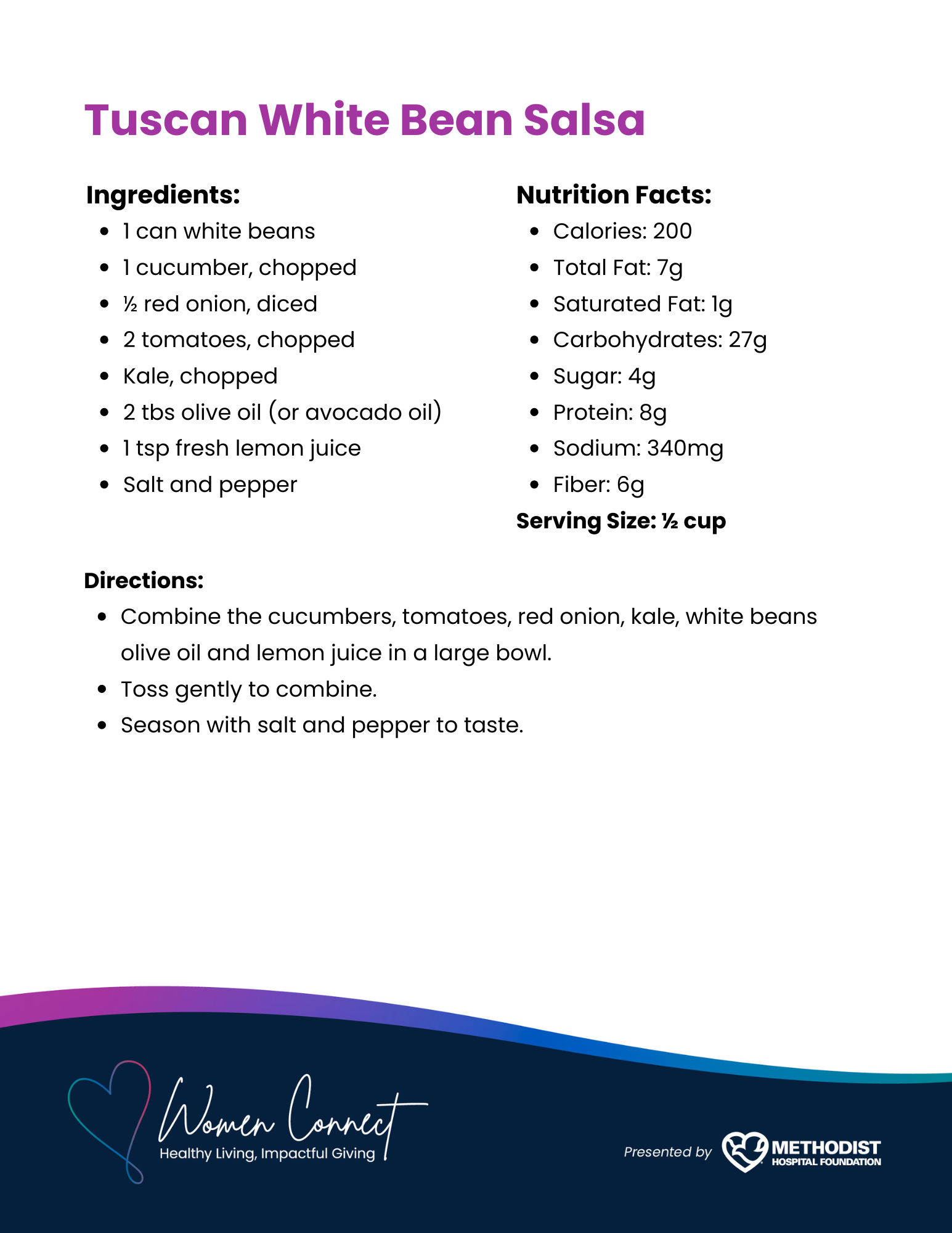
Recipes from our Pain Points event
Click on each image below for recipes featured at our event. You can also download them here.

Impactful Giving
Help patient overcome hurdles to healing!
Our Chronic Pain event supported the Methodist Equipment Loan Program, a recycle and reuse program that provides free home medical equipment to patients in need.
It's not too late to donate! Your gifts – of any size – will impact lives one walker, wheelchair and crutch at a time.
As a special thank-you, everyone who donates $30 or more will receive a Methodist Sling bag!
Have a friend or family member who would be interested in Women Connect?
Please forward this link so they can learn more: MethodistHospitalFoundation.org/WomenConnect